…no matter what you do. No matter how well you eat, how much you rest, sometimes having fibromyalgia and IBS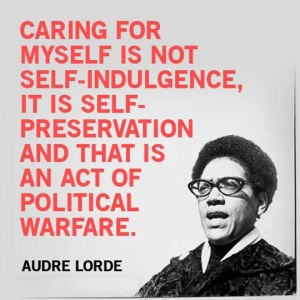 just kicks your butt (and your gut). Your body is at war with itself, and the only way you can survive is to retreat—at least for a while.
just kicks your butt (and your gut). Your body is at war with itself, and the only way you can survive is to retreat—at least for a while.
For the past few days I’ve been having a hard time getting my GI tract to settle down. I thought I was sticking to low-FODMAP foods, but I was still feeling lousy after every meal. The discomfort wasn’t only lower GI, either—I was nauseated, even by things that I usually tolerate pretty well, like oat cereal and (sadly) my treasured one cup of morning coffee. Then I realized I’d probably been eating out too much—even though I thought I was making good choices from my personally vetted list of menu items at “safe” restaurants. The truth is, no matter how innocuous someone else’s cooking seems, you can never be sure exactly what’s in it. Sigh. So it’s time to go back to basics—home-cooked, reliable, and (again sadly) pretty bland meals—at least until the gut calms down again.
So what are my standbys for days when the tummy is extra temperamental? For breakfast, brown rice with warm almond milk and a pinch of brown sugar and cinnamon. Half a ripe banana. For lunch, a small turkey sandwich with a bit of mayo on gluten-free bread. For dinner, plain grilled chicken breasts and baby potatoes or carrots roasted with a little olive oil. And, to drink, my favorite nausea-reducing beverage, Ginger Green Tea. I keep a jug of this in the fridge most of the time. It couldn’t be simpler to make: just put two tea bags each of 100% ginger tea and decaffeinated green tea in a two-quart/liter pitcher or bottle and fill with cold (preferably filtered) water. Cover the pitcher and refrigerate. The tea is ready to drink in about two hours. (If the brew is too gingery for your taste, use only one ginger tea bag.) I like Traditional Medicinals ginger and Bigelow’s green decaf, but of course any brands will do. 
Fight on.